Lipoprotein(a)
This test should be measured in every human, but many doctors don't know about it
Lipoprotein(a) (pronounced “Lipoprotein little a”) or Lp(a) for short, is an extremely important ApoB100 containing lipoprotein that is made in the liver, which was previously introduced in Assessment of Cardiovascular Disease (CVD) Risk, Part 1.
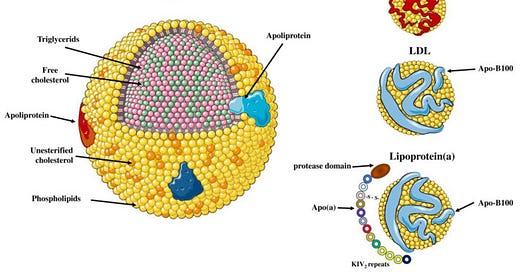
In structure, Lp(a) is extremely similar to LDL, except that it has an attached glycoprotein called Apolipoprotein(a) or Apo(a), which has several domains:
Kringle protein repeats, made of various types of plasminogen-like kringle IV, called KIVs, and result in varying lengths of the Apo(a) protein. These vary in number between 10-50, and are controlled by the LPA gene. There is an inverse correlation between the number of KIV repeats and the concentration of Lp(a) in the blood. In other words:
If you have high Lp(a), you will have shorter Apo(a), due to less KIV repeats.
If you have low Lp(a), you will have longer Apo(a), due to more KIV repeats.
An inactive proteinase-like domain, which is similar to the protease domain of plasminogen, a protein involved is involved in blood clotting.
Image source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9918959/
The amount of Lp(a) in each individual is genetically controlled by the LPA gene. Numerous SNPs (small nucleotide polymorphisms — which are basically subtle documented genetic differences) have been found that correlate with Lp(a) levels and CVD risk. If you have ever had genetics done through 23andMe or a similar service and download your raw data, you can browse the data using a service like Promethease.
Lp(a) levels vary widely. Some people have undetectable levels, and some people have levels up to 200 mg/dL or higher.
Why is Lp(a) so bad?
Elevated levels of Lp(a) have been shown to be a significant risk factor for atherosclerosis and CVD, and in a simple way can be thought of as a bad version of LDL. Elevated levels are also a risk factor for the development of aortic valve stenosis.
Reasons why Lp(a) is significantly more atherosclerotic than LDL (despite the fact that there are significantly less Lp(a) particles in the bloodsteam) include:
Lp(a) can more easily attach to the arterial wall than LDL due to its structure.
Promotes the recruitment of inflammatory cells to the vessel wall.
Is associated with oxidized phospholipids, which when present in high levels can contribute to atheromatic actions such as foam cell formation, inflammation, and plaque instability
Affects the stability of atherosclerotic plaques, by interacting with metalloproteinases and elastases, making them prone to rupture.
Affects endothelial function, making more permeable, and increasing reactive oxygen species.
Results in increased thrombosis, related to similarities to plasminogen.
Honestly, this is just a few of the ways that Lp(a) is bad.
Unfortunately, many doctors, including cardiologists never check or don’t know about Lp(a).
Because Lp(a) levels are mainly driven by genetics, a person typically only needs to check levels once in their life.
If your levels are over 40-50 mg/dL, then you have some increased risk of CVD.
Unfortunately, it’s not clear that lowering levels of Lp(a) will improve cardiovascular disease outcomes (even though it seems intuitive that it should).
Unfortunately, there are extremely limited ways to lower Lp(a) at the current time.
The most hopeful way for people who have very high levels of Lp(a) (typically over 150 mg/dL) are medications that will interfere with RNA expression of the Apo(a) gene. These are still in development.
Testosterone replacement therapy in men or estrogen replacement in women has been shown to lower Lp(a) levels in small to moderate amounts. There is no data as to whether this method improves cardiovascular outcomes.
Niacin is commonly used to lower Lp(a), but unfortunately it has not been shown to improve cardiovascular outcomes. Niacin may result in increased insulin resistance, which could negate the Lp(a) and other lipid lowering effects.
Ubiquinol does appear to have some limited ability to lower Lp(a), and is something I suggest L-carnitine also has some ability to lower Lp(a).
It is possible do do lipoprotein apheresis (basicially using a machine to remove your lipids from your bloodsteam and put everything else back in), but it has to be done 1-2 weeks, and isn’t widely available.
Other things to do if you have elevate Lp(a)
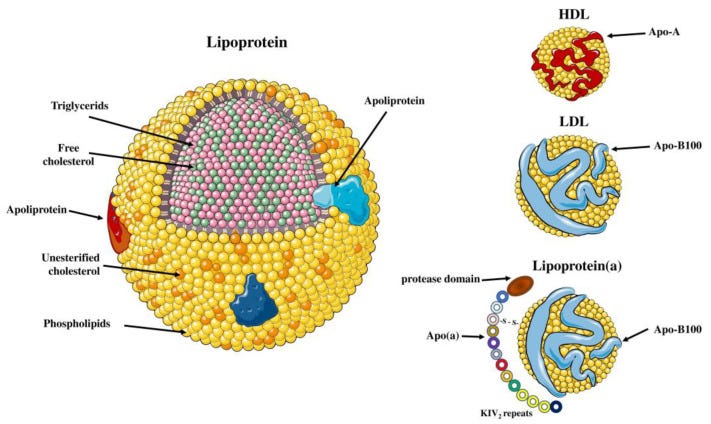
If you find out that this is something you have, then you want everything to be in the “Optimal” part of my guide, somewhat irregardless of how you get there.
This is because there is an additive effect of having elevated LDL and ApoB on top of having Lp(a). Despite what I wrote on the last section, we can’t reliably lower Lp(a), so we have to focus on what we can control.
As before, I generally try to avoid statins at first for prevention, and it should be noted that occasionally statins will increase Lp(a) levels — but this is very inconsistent, so you do need to monitor. Other methods to consider first from a pharmaceutical standpoint generally include ezetimibe and PCSK9 inhibitors. A more complete look at all of this will come in a later post.
One caution: avoid HGH and growth hormone secretagogues
Unfortunately, while TRT and estrogen replacement therapy can be helpful for lowering Lp(a) levels, we have also discovered that using exogenous HGH and growth hormone secretagogues such as ipamorelin and iermorelin can increase Lp(a) levels. If you do use any of these agents, I would suggest that you monitor Lp(a) levels.
In closing
Make sure you get checked to see if you have elevated Lp(a)!!!
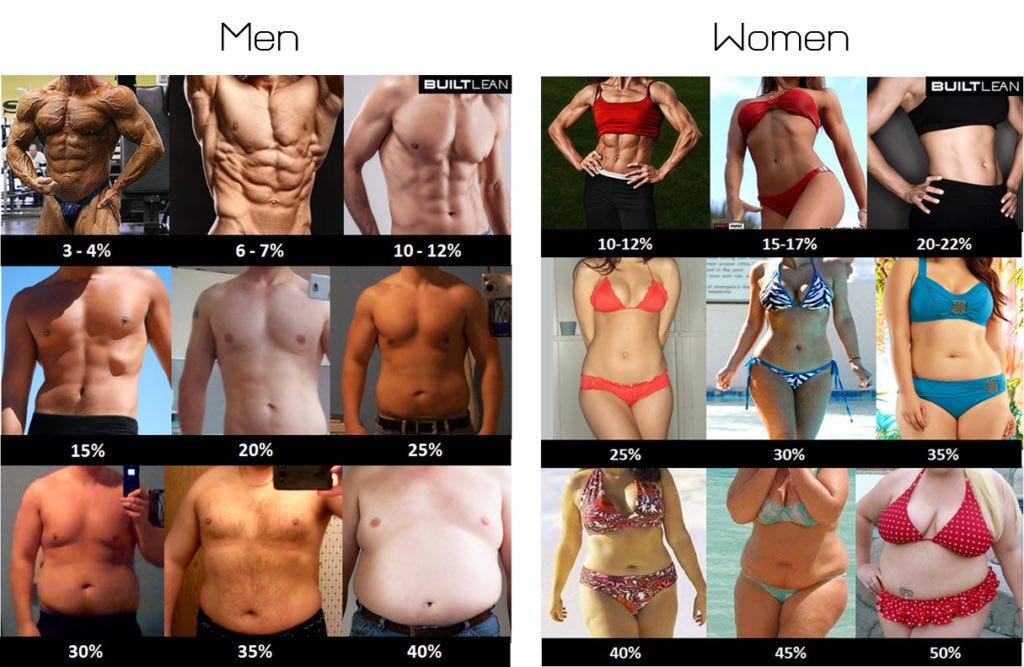
If you do find out that you have elevated Lp(a), your main goals at this time would be to get your lipids in the optimal range on the above chart, along with doing all of the other things for your health that we talk about all the time on Twitter, with probably the most important being lowering your bodyfat to a healthy range (under 15% and preferably less for men, under 22% and sometimes less for women) and doing zone 2 cardio.


Would >40 be “elevated Lp(a)” or is that >50? Understand that cutoff points are somewhat arbitrary and risk increases with a higher numbers, eg 70 significantly riskier than 50.