Intro
Cardiovascular disease is the number one cause of death in humans worldwide, representing about 31% of all deaths worldwide.
Unfortunately, humans are short-term thinkers in general, and this isn’t really a fun topic unless you’re someone like me, if you want to be elite you need to know this.
Part 1 of this post will focus on pathophysiology and risk factors for CVD. In part 2, we’ll talk most about lab assessment (which is easier for some categories than others).
Definitions and Categories of Risk Factors
The vast majority of CVD is caused by atherosclerosis, which is when the arteries that supply blood to important things like your heart, brain, and other organs become narrowed due to accumulation of fatty lipid deposits, called plaques.
The main factors that affect your risk of developing atherosclerosis are:
Lipids
Endothelial health
Inflammation
First, I’m going to briefly cover #2 and #3, since most people think this is only about the lipids, but there is obviously more to it. Since this will get somewhat detailed quickly, focus on understanding the definitions of the words in bold and important statements in italics.
Endothelial Health
Endothelial cells are the individual cells which make up the endothelium, which lines the inner surface of the blood vessels. It plays a critical role in regulating blood flow, controlling blood pressure, and preventing the formation of blood clots. In simple terms, the endothelium is the inner lining of the blood vessels that helps to maintain healthy blood flow and prevent the formation of clots.
In terms of development of atherosclerosis, damage to the endothelium makes It easier for lipids to pass into the vessel wall (which has multiple layers), and form a plaque. Later, this damaged endothelium makes cholesterol plaques more prone to rupture, which the body responds to with a clot, and can catastrophically block an artery when a cholesterol plaque ruptures.
The biggest factor to think of when looking at endothelial health is blood sugar. High blood sugar damages endothelial cells by causing excessive production of free radicals, which are highly reactive molecules that cause damage to tissues. Sometimes free radicals can be good, such as when they are produced by the immune system to fight an infection or destroy cancer cells, but in an age where we have sanitary conditions and hopefully go the majority of our lives without significant cancer, we don’t need them most of the time.
While a certain amount of free radicals are normal byproducts of metabolism, which our body is built to handle, it is when they become excessive that they damage tissues such as the endothelium.
In the cause of hyperglycemia, the high levels of blood sugar result in glucose molecules attaching to certain proteins and lipids, forming a type of free radical called advanced glycation end products (AGEs). Free radicals will also damage certain proteins in the body, which are called advanced oxidation protein products (AOPPs), which further damage the endothelium. Overall, this is a terrible feedback loop where damage gets amplified.
Other causes of free radicals that affect the endothelium generally include smoking, exposure to pollution, or radiation. (Nerdy sidebar: very few astronauts have been exposed to deep space radiation, but those that have developed much more significant and earlier atherosclerosis than astronauts that have remained in low-earth orbit. https://doi.org/10.3389/fcvm.2021.631985 Elon, if you’re reading this, hit my DMs).
The other important risk factor that affects endothelial health is hypertension (elevated blood pressure). High blood pressure has negative impacts on endothelial health via several mechanisms:
Direct mechanical stress on endothelial cells, resulting in damage
Resulting production of reactive oxygen species (ROS), which can cause additional oxidative stress and damage.
Damaged endothelial cells become dysfunctional, and less able to regulate vascular tone and blood flow, which can lead to vasoconstriction with decreased blood flow, which contributes to atherosclerosis by decreasing delivery of oxygen and nutrients to the endothelium, further worsening damage.
By activating the renin-angiotensin-aldosterone system (RAAS), which can lead to the production of angiotensin II, a potent vasoconstrictor that can also stimulate the production of ROS and pro-inflammatory cytokines (discussed more below).
Inflammation
To avoid confusion, inflammation defined as activation of the immune system. While the immune system technically involves many parts, when discussing its relation to atherosclerosis, we’re generally focused on a certain cell type called macrophages which is involved in chronic inflammation.
Macrophages are a type of white blood cell are that normally engulf (consume by surrounding) bacteria, dead cells, and other harmful substances from the body. (If you’re looking at literature about this, you might come across monocytes as well. These are precursors to macrophages that are usually flowing through the bloodstream).
In the context of atherosclerosis, macrophages will engulf lipid particles that have passed the endothelium to the point that they become overloaded an look foamy under a microscope (at which point we literally call them “foam cells”). Foam cells are the precursors of plaques, and as these cells accumulate and grow, they can form a mass of cholesterol, calcium, and other substances within the artery wall. This process is called plaque formation.
Chronic inflammation can be increased by certain cytokines, which are signaling molecules that the immune system uses to communicate. Some of the most important cytokines involved in chronic inflammation that relates to atherosclerosis are TNF-alpha, IL-1, and IL-6. These cytokines are elevated due to obesity, smoking, diabetes, as well as chronic infections.
Lipids
My current stance on the importance of lipids in atherosclerosis is this:
ApoB containing lipoproteins (primarily LDL) are necessary for the development of atherosclerosis, but not always sufficient on their own for development of the disease.
Why do I say this?
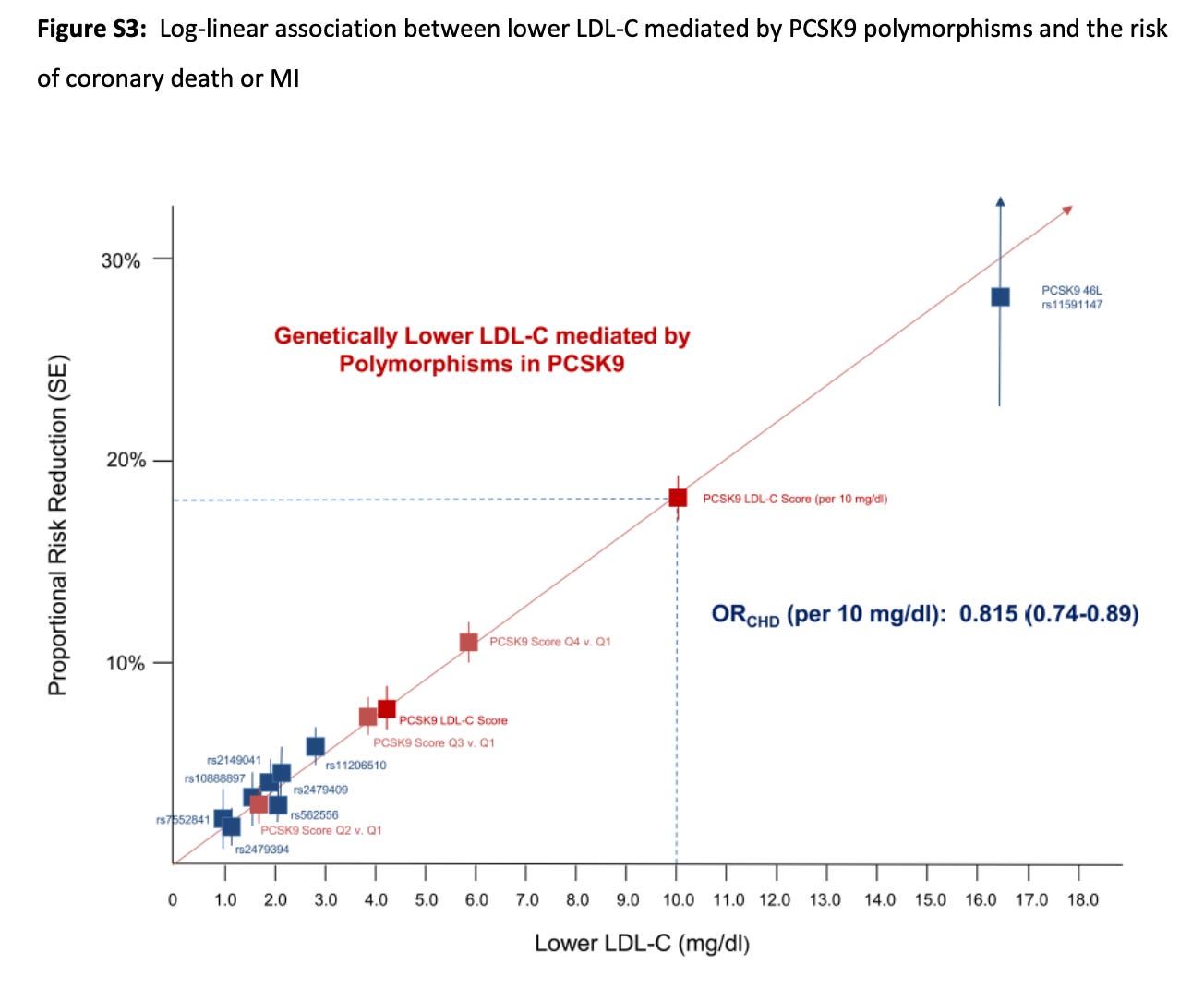
In people with genetically extremely low LDL levels (due to nonsense mutations in PCSK9), end up having an extremely low lifetime risk of CVD (source is the supplemental appendix to the above article). This supports the idea that low LDL levels are important in the development of atherosclerosis (as opposed to a potential effect of a cholesterol lowering medication that is independent of the lipid-lowering effects).
This statement helps explain why some people (although not many) with high LDL levels (e.g., >190 mg/dL) are able to avoid the development of atherosclerosis well into their elder years — they likely have good endothelial health and low levels of inflammation, which keep ApoB containing lipoproteins from passing through their endothelium. (From my experience, this is uncommon)
Similarly, this statement helps explain why some people with low LDL (e.g., <70 mg/dL) will still develop atherosclerosis, sometimes at an early age. Many of these people have poor endothelial health and high levels of inflammation, due to conditions such as obesity, diabetes, high blood pressure, and smoking.
Why do I keep saying ApoB containing lipoprotein?
Because the ApoB (actually ApoB100, since there is a ApoB48 protein as well, but since we mostly care about ApoB100, I’ll continue to just refer to this as ApoB) containing lipoproteins are the ones that are associated with atherosclerosis.
These are:
LDL ("Low density lipoprotein”) - typically 90-95% of total ApoB lipoproteins
VLDL (“Very low density lipoprotein”)
IDL (“Intermediate density lipoprotein”)
Lp(a) (“Lipoprotein little a”)
What is a exactly is ApoB?
ApoB is an apoprotein, which is one of these amazing molecules that allow cholesterol (something that normally cannot be dissolved in liquid) to become soluble and dissolve in the bloodstream, allowing it to be transported through the body.
Once Apoprotein is bound to lipids, we call it an apolipoprotein. (Image source)
Why do levels of ApoB containing lipoproteins matter?
Over time, we have seen a direct correlation with ApoB levels and the risk of atherosclerosis. As explained above, this isn’t a perfect correlation.
To go into even more detail, we have learned that the number of ApoB particles in the bloodstream is even more important than the concentration.
The reasoning for this is fairly simple: the more often you have a particle hit the endothelial wall, the more likely it is to pass the wall. It’s just statistics.
Particle numbers are measured in nmol/L. A mole is 6.02 x 10^23, so a nanomole (nmol) is one billionth of this, or 6.02 x 10^14.
Lipid concentrations are generally measured in mg/dL (milligrams per deciliter).
Unfortunately, it’s near impossible at this time to find a lab that will report ApoB particle numbers, so in general, we’re looking at LDL particle numbers.
LDL-C vs LDL-P
At some point, you’ve probable seen the abbreviations:
LDL-C - this is LDL concentration (measured in mg/dL)
LDL-P - this is LDL particle numbers (measured in nmol/L)
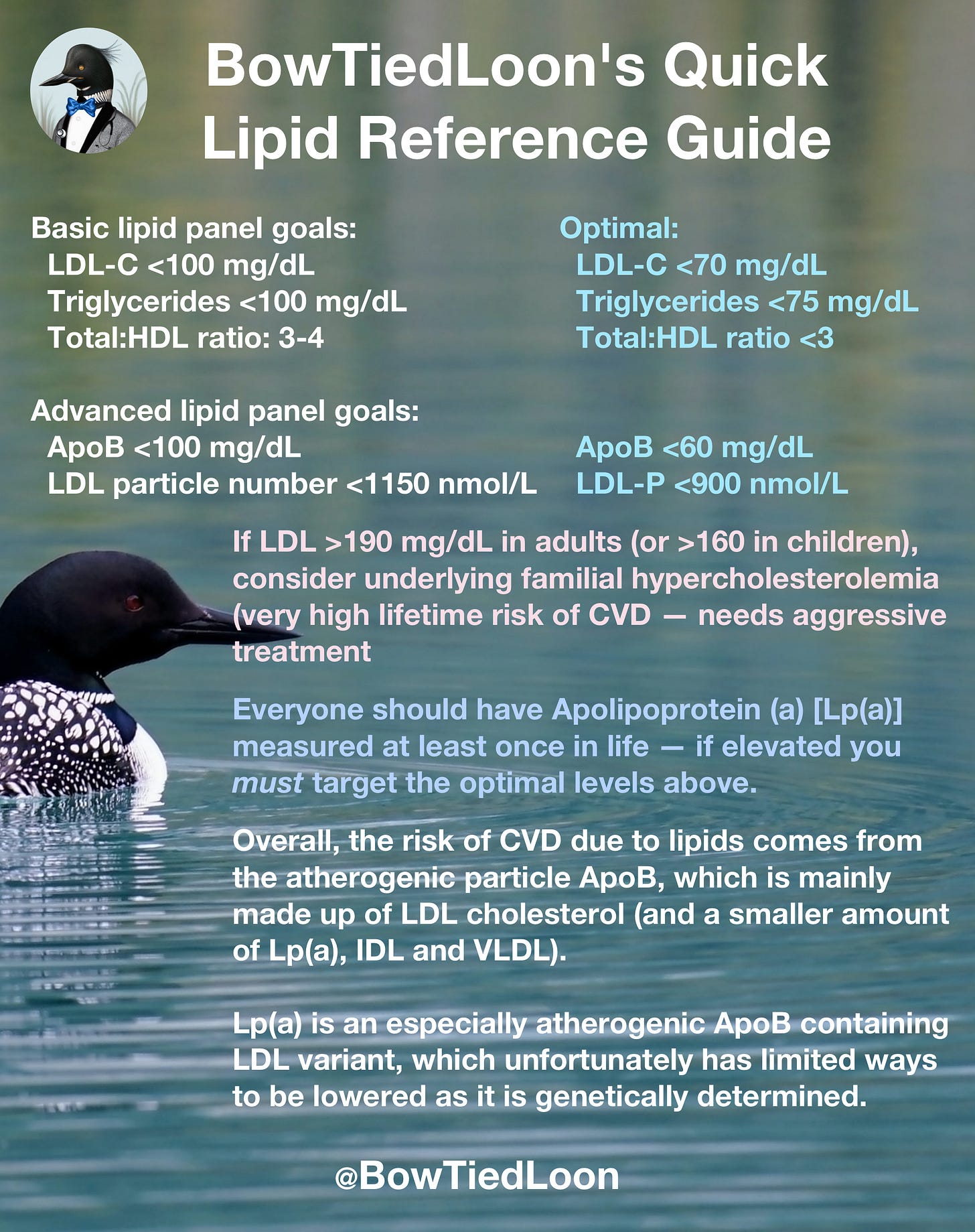
Lipid goals:
I’ve posted this graphic before, but if you’ve read through this longer post, you’ll now hopefully understand why I list the following under “Advanced lipid panel goals”.
More specifics regarding these labs to come in part 2…




Tks for the informative post. Interested in your thoughts on 1) tests/ranges for inflammation markers, 2) test profiles for which you recommend following the “optimal” goals vs baseline goals, 3) actions/habits/behaviors that may move these numbers and lower risk (in addition to lose weight don’t smoke eat well and exercise lol). Niacin?