Assessment of Kidney Function
Creatinine, GFR, Cystatin C, and BUN
In this post, we’re going to cover the main tests used to measure kidney function.
Creatinine and GFR (glomerular filtration rate).
Creatinine is a waste product that is produced by muscle metabolism and excreted by the kidneys. The level of creatinine in the blood can be used as a marker of kidney function because the kidneys are responsible for filtering and removing creatinine from the bloodstream. The amount of creatinine is typically expressed in mg/dL.
Creatinine levels can be affected by several factors besides kidney function, most commonly: 1) muscle mass, 2) dietary intake of protein, 3) dehydration, 4) medications such as ARBs/ACE inhibitors, and NSAIDs, 5) creatine supplementing (this is not harmful to kidneys but can affect lab interpretation; more discussion below).
GFR is a measure of the rate at which the kidneys are filtering the blood to remove waste products. The units used to express GFR is typically mL/min/1.73m², which is milliliters of blood filtered per minute, and then divided by an arbitrary adult body surface of area so that these values can more easily be compared among individuals. (For the most part, it’s easier to consider this just to be mL of blood filtered per minute).
In general, as kidney function decreases, creatinine will build up to higher levels, which indicates a decrease in GFR.
There are a variety of calculations used to determine GFR, which is beyond the scope here. Most of these calculators can only report that your GFR is 60 mL/min or higher, most healthy men will have a GFR of 100-130 or more, and most healthy women will have a GFR of 90-120 or more.
Additionally, it’s important to understand that increases in creatinine logarithmically affect GFR, whereby each unit of increase in creatinine from baseline indicates an additional 50% decline in GFR. Because creatinine is affected by several factors as mentioned above, it is helpful to measure several values over time to establish your baseline value for comparison.
Once we know your baseline creatinine, we can estimate how changes in your creatinine affect your GFR. Hopefully this makes the most sense using an example — you can fill in your own creatinine for “x” below:
With this in mind, you can see that if someone has a baseline creatinine of 0.75, if their creatinine increases to 1.5, they have an 50% decrease in their kidney function. If this happens over a short period of time, we call this acute renal failure (ARF) or acute kidney injury (AKI).
When ARF or AKI occurs, we divide the causes into pre-renal causes (mostly problems with decreased blood flow (low blood pressure to the kidneys, such as from dehydration, bleeding, or poor heart function), intrinsic-renal causes (direct damage to the kidneys, such as from medications, kidney infection (pyelonephritis), or diseases such as glomerulonephritis), or post-renal causes (blocking urinary outflow from the kidneys, such as from a kidney stone or mass). The approach to ARF/AKI is well beyond the scope of this guide, but there are numerous guides to this available in articles and textbooks.
False elevations in creatinine can occur from recent ingestion of a massive amount of meat, or from a massive muscle injury (such as a severe crush injury or rhabdomyolysis — although each of these can directly cause renal failure as well).
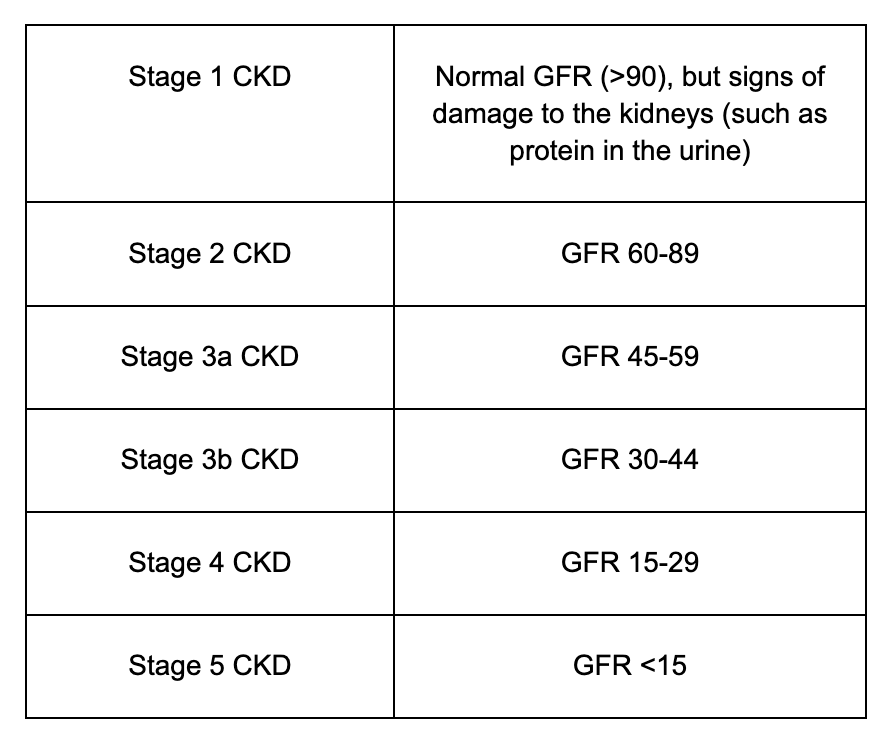
When GFR is chronically reduced, we call this chronic kidney disease, or CKD. CKD is typically divided into stages:
In general, a GFR above 60 is considered normal. This said, if you have a CKD stage 3a (GFR >45), you can live a fairly normal life (although you should be doing everything you can to protect your kidneys, and likely following with a nephrologist).
Stage 3b CKD and beyond is when people really start to to have problems, and as people approach stage 4 CKD, they often need to start considering dialysis and/or kidney transplant.
Despite all of the above talk of reasons that creatinine can be elevated, the most common reason that I see someone’s creatinine above baseline is simple dehydration. Since a high percent age of people do their labs fasting in the morning, they tend to be dehydrated from water loss overnight. We can often get some clues about dehydration by looking at the BUN.
As mentioned briefly above, the supplement creatine can affect creatinine levels. I’ve mentioned this numerous times before on my Twitter account, but all of you should be taking creatine 5g/day (or more), due to its many benefits on muscle and brain function. Because creatine is converted to phosphocreatine (which is spontaneously converted to creatinine), it can increase measurements of serum creatinine and make estimates of true renal function and GFR more challenging. It does not actually damage the kidneys or cause a decrease in renal function or GFR.
Cystatin C.
Cystatin C is a newer test used to measure kidney function and calculate GFR.
Similar to creatinine, cystatin C is filtered by the kidneys, so increasing levels are indicative of worsening kidney function.
Unlike creatinine, cystatin C is not affected by muscle mass or diet, which makes it helpful for weightlifting/bodybuilding types who tend to have more than the “standard” amount of muscle mass or eat closer to 1g of protein per pound of bodyweight.
The normal functions of cystatin C in the body are 1) regulation of certain proteases that breakdown proteins in the body, 2) has antimicrobial properties, and 3) is involved in the activation of certain immune cells.
Because of the above normal functions, cystatin C is affected by infection and other inflammatory conditions, such as obesity, so these need to be taken into consideration when looking at results.
BUN (Blood Urea Nitrogen)
BUN comes from the byproduct of protein metabolism as it is metabolized by the liver in the urea cycle. Similar to creatinine and cystatin C, increasing BUN levels can be suggestive of worsening kidney function.
In healthy individuals, BUN is a good marker of how much blood flow is currently going to the kidneys, and is more sensitive to dehydration than creatinine.
BUN can be increased by high protein diets and urinary obstruction (blockage of urine leaving the kidneys) are other known causes of BUN increase.
BUN is generally more useful when combined with creatinine to look at the BUN/creatinine ratio.
Most labs use an upper limit of 20 for the BUN/creatinine ratio, although I tend to suspect some degree of dehydration in people who are in the 15-19 range as well (especially if they don’t eat a high protein diet).
Causes of a high BUN/creatinine ratio (generally >20) include:
Kidney disease. While usually this is better detected by worsening creatinine/GFR, when the BUN levels significantly increase (often to the 80-100 range), patients will have signs of uremia, which include nausea, metallic taste in the mouth, muscle cramps, and itching (among other symptoms).
Anything that decreases blood flow to the kidney, such as dehydration, congestive heart failure, or bleeding.
Increased protein intake in the gut. Generally this is due to diet. Of note, an elevated BUN/creatinine ratio can be a subtle clue to GI bleeding because the blood in the GI tract is digested and will significantly increase BUN.
Hyperthyroidism. This is due to elevated thyroid function causing an increase in protein catabolism (which increases BUN), and decreased creatinine (due to increasing GFR).
Cortisol excess, either due to Cushing’s syndrome (usually due to the pituitary producing too much ACTH, which causes the adrenals to produce too much cortisol) or by taking corticosteroid medications such as prednisone or methylprednisolone. In either case, the result is increased protein catabolism, which increases BUN.
Causes of a low BUN/creatinine ratio (generally <6) include:
Low protein intake in the diet.
Advanced liver disease, where the liver cannot produce urea which results in lower BUN levels.
Hypothyroidism, for the opposite reasons from hyperthyroidism (listed above).
Rhabdomyolysis (excessive breakdown of muscle tissue). Due to the massive release of creatinine into the bloodstream from muscle breakdown, the BUN/creatinine ratio is typically low.
Neither of these lists is exhaustive, but both cover the most common causes we might see.
Actionable Advice
For most people, assessment of kidney function with the usual labs in a basic metabolic panel or comprehensive metabolic panel will be sufficiency, as creatinine and BUN are included.
If you’ve never had your labs checked before, but are more muscular or eat more protein in your diet than someone in the normal population, you may was to obtain a cystatin C as well. You may also want to check a cystatin C if your creatinine comes back unexpectedly high.
Most people don’t need to monitor cystatin C regularly once they have established that they have a normal GFR (based on cystatin C) and correlated this to find their baseline creatinine levels.